Get Your Insurance Appeal Approved Fast
Beat automated denials with a proven packet your doctor can submit today. Works for prescription weight management and diabetes medications.
30-Day Money-Back Guarantee · Instant Download

If You Were Denied, It Wasn't Your Fault
Your doctor prescribed it. You need it. But insurance said no. The truth? A computer algorithm flagged your case before any human even looked at it. You're not being judged on your health—you're being filtered by policy code triggers designed to make you give up.
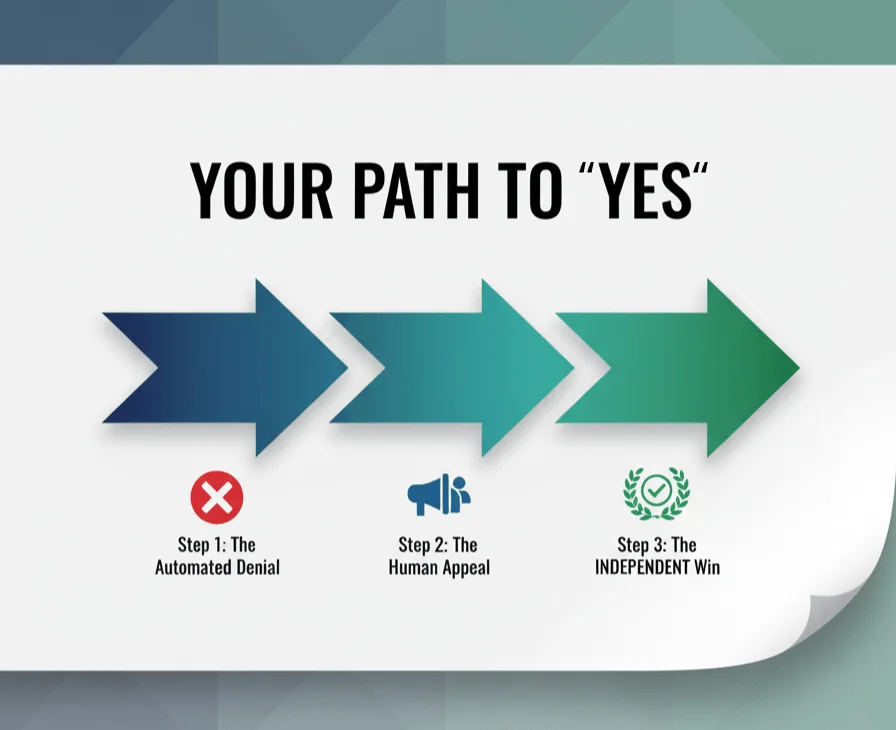
How Appeals Actually Get Approved
Follow the step-by-step roadmap from the 31-page Guide
Use the correct sequence of documents
Include only the insurer-required medical details
Submit cleanly using the Cover Sheet
Follow your 30-day timeline and call prompts
Escalate correctly if needed
Add the right exception request when required
The 31-Page Appeal Guide: Your Core Playbook
A clear, step-by-step walkthrough of the entire approval process—from decoding your denial to building the packet, submitting it correctly, following deadlines, and escalating when needed. Everything else in this toolkit supports this Guide.
Everything You Need to Build an Approval-Ready Appeal
Appeal Packet Templates
- • Letter of Medical Necessity
- • Step-Therapy Exception
- • Formulary Switch Request
- • Documentation forms (BMI history, comorbidities, prior treatments)
- • Employer Benefits Exception (HR)
Follow-Up Engine
- • 30-day tracker & deadline prompts
- • Phone scripts (insurer, clinician, HR)
- • Email & portal message templates
- • Submission cover sheet for clean packets
Strategy Guide
- • Identify your true denial reason
- • Know when to escalate (peer-to-peer, external review)
- • Navigate formulary and coverage rules
- • Decide what to send first, second, and third
From the Creator
I built this toolkit because I went through the denial process myself. When my own insurer rejected a medically necessary treatment, I spent weeks digging through policies, appeal codes, and state-level rules. After multiple rounds of appeals, I finally won.
I took everything I learned — the strategy, the documentation order, the templates that worked, and the follow-up scripts — and turned it into this toolkit so you don't have to start from scratch.
What's Behind the Toolkit
Built from patterns in 50+ real denial letters
Includes insurer-required medical elements
Structured using best practices from successful appeals
Designed so your doctor can submit in minutes
Get Approved Faster—Without Guesswork
Everything you need to build an approval-ready appeal packet.
Educational resource – not medical or legal advice. Use your plan's secure portal or fax for PHI. Results vary by plan design, medical policy, and documentation completeness. Brand names belong to their owners; no affiliation implied.